Stronger ASC Billing, Fewer Denials, Better Collections
You’re moving fast, multi-procedure cases, device costs, tight turnarounds. Your payments should move just as fast. With reliable ASC billing services, you get fewer denials, steady cash flow, and clear visibility into every dollar.
- 98%+ First-Pass Acceptance
- Charge Entry & Scrubbing in 24 hours
- 40–60% Fewer Rejections
- 24–48 hr Denial Resubmission



Complete RCM Support That Pays Off Every
Month
Focused work on >60/90-day bucket, payer-specific follow-ups that pull cash forward for ASC medical billing.
Daily ERA/EOB posting, line-by-line checks, unapplied cash resolved, clean books all year round.
Faster enrollments and updates so surgeons and new service lines can bill immediately in ASC billing services.
Detailed audits help providers recover 20–35% more revenue by spotting and fixing recurring issues.
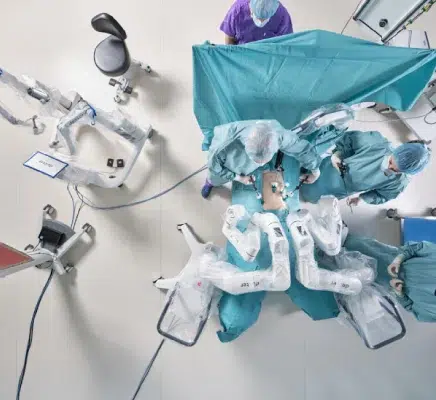
The Roadmap to Stronger Ambulatory Surgical Centers Billing
High-velocity cases deserve high-velocity payments. We start with pre-op eligibility and authorizations so your claims are ready the moment the case closes. Op notes, devices, and supplies are captured the same day; charge entry is completed within 24 hours.
Claims go out daily with ASC-specific edits (modifiers, multiple-procedure rules, packaged services). Denials are analyzed and corrected within 24–48 hours. Posting happens every daywith line-level reconciliation, no unapplied cash, no mismatches.
Your outcomes: 97%+ first-pass acceptance, 40–60% drop in rejections in month one, and $25K–$70K commonly uncovered in the first two weeks, no-risk audit. Leadership sees real-time dashboards, what’s paid, what’s pending, and what needs action.

Challenges That Slow Down Ambulatory Surgical Centers
- Wrong payer rules for multiple-procedure discounting and packaged services
- Delayed prior auths for scopes, devices, and high-cost meds
- Professional vs facility splits mishandled across specialties
- A/R 60–90 days with weak follow-ups
- Medicare ASC fee schedule rules are not applied consistently
- Limited reporting, no line-level view of what’s paid, pending, or stuck
How We Fix It Effectively
We align your workflows to ASC medical billing rules with precise coding, device/implant capture, and payer-specific edits before a claim ever goes out. Prior auths are handled upfront, claims are submitted daily with no backlog, and denials are worked the same day.
Our RCM Services
Eligibility & Benefits Verification
We verify coverage, copays, deductibles, and plan limits pre-op so ASC billing starts clean and avoids retro denials.
Prior Authorizations
We manage pre-auth for scopes, devices, biologics, and high-cost meds—reducing delays in ASC medical billing services.
Charge Capture & Coding
Accurate CPT/ICD-10 with ASC-specific logic (NCCI edits, device/implant capture) for compliant Ambulatory Surgical Centers Billing.
Claim Submission & Tracking
Same-day submission with payer-specific edits; proactive tracking keeps ASC billing services moving without stalls.
Denial Management & Appeals
Root-cause analytics, quick fixes, and written appeals, tight feedback loops that protect ASC medical billing revenue.
Zero-Balance Audit Recovery
We re-audit “closed” claims to find missed modifiers, underpayments, and device pass-throughs often lost in ASC billing.
Trusted by Medical Practices Nationwide
Honest experiences from the practices we’ve partnered with. See how we’ve improved collections and reduced stress for them.



