Medical Billing Services: 3 best Strategies for Maximizing Revenue
What Are Medical Billing Services? Medical billing services are outsourced services that handle the complex administrative process of submitting and following up on medical insurance claims. These services include tasks such as claim submission, patient billing, and insurance verification.
How medical billing services help healthcare providers: Medical billing services help healthcare providers to streamline their billing process and ensure accurate and timely payments from insurance companies. This, in turn, allows healthcare providers to focus on providing quality patient care and growing their practice.
Table of Contents
ToggleThe Benefits of Outsourcing Medical Billing
Understanding an Itemized Bill from a Hospital
What is an itemized bill? When you receive a bill from a hospital, it’s important to review it carefully to make sure you understand all of the charges. An itemized bill is a detailed breakdown of all the charges associated with your hospital stay, including room and board charges, medication charges, lab and imaging fees, and surgery and procedure fees. Understanding your itemized bill can help you avoid overpaying for services you didn’t receive and catch any billing errors.
Components of an Itemized Bill
An itemized bill from a hospital typically includes charges for room and board, medication, lab and imaging fees, and surgery and procedure fees. Room and board charges cover the cost of your hospital room, meals, and other amenities. Medication charges include the cost of any drugs you were prescribed during your stay. Lab and imaging fees cover the cost of any lab tests, X-rays, or other diagnostic tests that were ordered. Surgery and procedure fees cover the cost of any surgeries or medical procedures you received during your hospital stay.
Room and Board Charges
Room and board charges are a significant part of any hospital bill, as they cover the cost of your room, meals, and other amenities. The charges can vary based on the type of room you were in, the level of care you received, and the hospital’s location. It’s important to review these charges carefully to ensure you were not overcharged and that the charges match the type of room you were in and the level of care you received.
Medication Charges
Medication charges on a hospital itemized bill include the cost of any drugs or medications you were prescribed during your stay. These charges can be significant, especially if you were prescribed expensive medications. It’s important to review these charges carefully to ensure you were not overcharged and that the medications were necessary for your treatment.
Lab and Imaging Fees
Lab and imaging fees cover the cost of any lab tests, X-rays, or other diagnostic tests that were ordered during your hospital stay. These charges can add up quickly, especially if you required multiple tests or if the tests were complex. It’s important to review these charges carefully to ensure you were not overcharged and that the tests were necessary for your treatment.
Surgery and Procedure Fees
Surgery and procedure fees cover the cost of any surgeries or medical procedures you received during your hospital stay. These charges can be significant, especially if you require complex surgeries or procedures. It’s important to review these charges carefully to ensure you were not overcharged and that the procedures were necessary for your treatment.

How are Charges Calculated?
Hospitals use a charge master to determine how much to charge for various services. The charge master is a list of prices for all the services provided by the hospital. Insurance contracts also play a role in determining how much you will be charged for services. Negotiated rates between your insurance company and the hospital can reduce the amount you owe. Payment policies, such as discounts for paying in cash or setting up a payment plan, may also affect the final amount you owe.
Requesting an Itemized Bill
Requesting an itemized bill is an important step in understanding your hospital charges. An itemized bill breaks down the charges for each service you received, making it easier to identify any errors or overcharges. It’s important to review the itemized bill carefully and dispute any incorrect charges.
Common Billing Errors to Watch For
Billing errors can occur when a hospital charges you for services you didn’t receive or when the charges on your itemized bill don’t match the services you received. Common billing errors to watch for include duplicate charges, incorrect billing codes, charges for services not rendered, and unbundling of charges.
Duplicate Charges
Duplicate charges occur when a hospital bills you for the same service more than once. These errors can be difficult to catch, especially if the charges are spread out over several pages of the itemized bill. It’s important to review your itemized bill carefully to ensure you were not charged twice for the same service.
Incorrect Billing Codes
Incorrect billing codes occur when a hospital bills you for the wrong service or procedure. This can happen if there is a mistake in the coding or if the code is outdated. It’s important to review your itemized bill carefully to ensure the billing codes match the services you received.
Charges for Services Not Rendered
Charges for services not rendered occur when a hospital bills you for a service or procedure that you did not receive. This can happen if there is a mistake in the billing or if the hospital is attempting to overcharge you. It’s important to review your itemized bill carefully to ensure you were not billed for any services you did not receive.
Unbundling of Charges
Unbundling of charges occurs when a hospital separates charges that should be billed together into separate charges. This can result in higher charges for patients and can make it difficult to compare prices across hospitals. It’s important to review your itemized bill carefully to ensure you were not overcharged due to unbundling of charges.
How to Dispute a Hospital Bill
If you find an error on your hospital itemized bill or believe you were charged too much, you can dispute the charges. Start by contacting the hospital’s billing department to explain the error or dispute the charges. If you are unable to resolve the issue with the hospital, you can file a complaint with your insurance company or seek help from a patient advocate. You may also consider filing a grievance with the state department of health.
Contacting the Billing Department
If you have any concerns about your medical itemized bill or insurance coverage, the first step is to contact the billing department of your healthcare provider. The billing department can help you understand your medical charges, provide explanations of benefits, and assist you with payment options. You can typically find the contact information for the billing department on your medical itemized bill or by contacting the healthcare provider’s main office.
When contacting the billing department, be prepared to provide your personal information and medical details, including the date of service and the type of treatment received. You may also want to have your insurance card and policy information on hand. Be clear and concise about your concerns, and ask questions if you do not understand something.
Filing a Complaint with your Insurance Company
If you are unhappy with your insurance coverage or the way your claim was processed, you have the right to file a complaint with your insurance company. You can typically find the contact information for your insurance company’s customer service or claims department on your insurance card or policy documents.
When filing a complaint, be sure to provide your personal information and policy details, as well as a detailed description of the issue you are experiencing. Be clear and concise about your concerns, and provide any relevant documentation or supporting materials. You may also want to ask for a reference number or case number so you can track the progress of your complaint.
Seeking Help from a Patient Advocate
A patient advocate is a professional who helps patients navigate the healthcare system and ensure they receive the best possible care. Patient advocates can help you understand your medical treatment options, communicate with healthcare providers, and resolve disputes with insurance companies or medical billing departments.
To find a patient advocate, you can contact your healthcare provider or hospital, or search online for local advocacy organizations. When working with a patient advocate, be sure to provide them with your personal information and medical details, as well as a detailed description of your concerns. Be clear and concise about your goals and expectations, and ask questions if you do not understand something.
Filing a Grievance with the State Department of Health
If you believe that your healthcare provider or facility has violated your rights or provided substandard care, you can file a grievance with the State Department of Health. Grievances can include complaints about medical errors, mistreatment, or neglect, among other issues.
To file a grievance, you can typically find the contact information for your state’s Department of Health on their website. Be prepared to provide your personal information and medical details, as well as a detailed description of the issue you are experiencing. You may also want to provide any relevant documentation or supporting materials. Be clear and concise about your concerns, and ask questions if you do not understand something. The Department of Health will investigate your complaint and may take action if they find evidence of wrongdoing.

Negotiating Your Hospital Bill
Negotiating your hospital itemized bill can help you reduce your out-of-pocket expenses and avoid unnecessary costs. You may be able to negotiate a lower rate for certain services, set up a payment plan, or qualify for financial assistance programs. It’s important to be proactive and communicate with the hospital billing department to explore your options. If you’re facing high hospital bills, there are several strategies you can use to negotiate a lower bill. Start by understanding your insurance coverage and researching average costs for procedures. You can also request a payment plan or explore financial assistance options, such as charity care or Medicaid.
Understanding Your Insurance Coverage
Understanding your insurance coverage is crucial when it comes to hospital billing. The first step is to carefully review your insurance policy to determine which services are covered and which are not. Most insurance policies have specific limitations and exclusions that you should be aware of, such as pre-existing conditions, deductibles, and co-pays. It is also important to find out if your policy requires pre-authorization for certain treatments or procedures. If you are unclear about your insurance coverage, contact your insurance provider or your hospital’s billing department for assistance.
Researching Average Costs for Procedures
Researching the average costs for procedures can give you a better understanding of what you should expect to pay for a hospital visit. Many hospitals and insurance companies provide pricing information for common procedures and treatments. This information can help you estimate your out-of-pocket expenses and plan for any financial obligations you may have. It is also important to note that costs can vary widely depending on the hospital and location. Therefore, it is advisable to compare prices at different hospitals and speak with your insurance provider about your options.
Requesting a Payment Plan
If you are unable to pay your hospital itemized bill in full, requesting a payment plan can help you manage your expenses over time. Many hospitals offer payment plans that allow you to pay your bill in installments over several months or years. Some hospitals may also offer zero-interest payment plans or discounts for paying in full upfront. It is important to communicate with your hospital’s itemized bill billing department and explain your financial situation to determine the best payment plan for you.
Exploring Financial Assistance Options
If you are struggling to pay your hospital bill, it is important to explore your financial assistance options. Many hospitals offer financial assistance programs for patients who are uninsured or underinsured. These programs may provide discounts, payment plans, or even free services to eligible patients. Some hospitals may also offer assistance in applying for Medicaid or other public assistance programs. It is important to speak with your hospital’s billing department and explain your financial situation to determine which programs you may be eligible for.
Tips for Reviewing Your Hospital Bill
To make sure you catch any errors or overcharges on your hospital bill, it’s important to review it carefully. Start by requesting an itemized bill and double-checking billing codes. Review your insurance explanation of benefits (EOB) to make sure the charges on your bill match the services you received. Finally, keep a record of all communication with the hospital and your insurance company.
Requesting an Itemized Bill
Requesting an itemized bill is an important step in understanding your hospital charges. An itemized bill breaks down the charges for each service you received, making it easier to identify any errors or overcharges. It can also help you verify that you received all the services listed and ensure that you are not being charged for any services you did not receive. You can request an itemized bill from your hospital’s billing department or by contacting your insurance provider.
Double-Checking Billing Codes
Double-checking billing codes is another important step in ensuring that your hospital itemized bill is accurate. Billing codes are used to identify the services and treatments you received and determine how much you should be charged. However, errors in coding can lead to overcharging or undercharging for services. It is important to review your itemized bill and ensure that the codes match the services you received. If you notice any errors, contact your hospital’s billing department or your insurance provider to request a correction.
Reviewing Your Insurance Explanation of Benefits (EOB)
Your insurance explanation of benefits (EOB) is a document that outlines the services and treatments that were covered by your insurance policy. It is important to review your EOB carefully and compare it to your hospital itemized bill to ensure that you were charged the correct amount. If there are any discrepancies between the two documents, contact your insurance provider or the hospital’s billing department to request a correction.
Keeping a Record of All Communication
Keeping a record of all communication is important when it comes to hospital billing. It can help you keep track of any discussions you have had with your hospital’s billing department or insurance provider and ensure that you have all the information you need to dispute any incorrect charges. It is also a good idea to keep a record of any bills, receipts, or other documents related to your hospital visit. This can help you stay organized and make it easier to review your charges and insurance coverage.

When to Seek Legal Assistance
In some cases, you may need to seek legal assistance to resolve a hospital billing issue. For example, if you believe you were the victim of medical malpractice, billing fraud, or denied insurance claims, you may need to consult with an attorney. Out-of-network billing can also be a complex issue that may require legal assistance.
Resources for Understanding Hospital Billing
If you’re struggling to understand your hospital itemized bill or need help resolving a billing issue, there are several resources available. Patient advocacy organizations can provide support and guidance, while state departments of health may have resources for filing complaints or grievances. Consumer reports and government websites may also have information on average costs for procedures and other helpful tips for navigating hospital billing.
Taking Control of Your Hospital Itemized Bill
Understanding your hospital itemized bill and knowing your rights can help you take control of your healthcare costs. By reviewing your itemized bill, disputing any errors or overcharges, and negotiating your bill when possible, you can avoid unnecessary expenses and make sure you’re only paying for the services you received. Advocating for better billing practices and staying informed about your rights and options can also help you protect yourself as a patient.
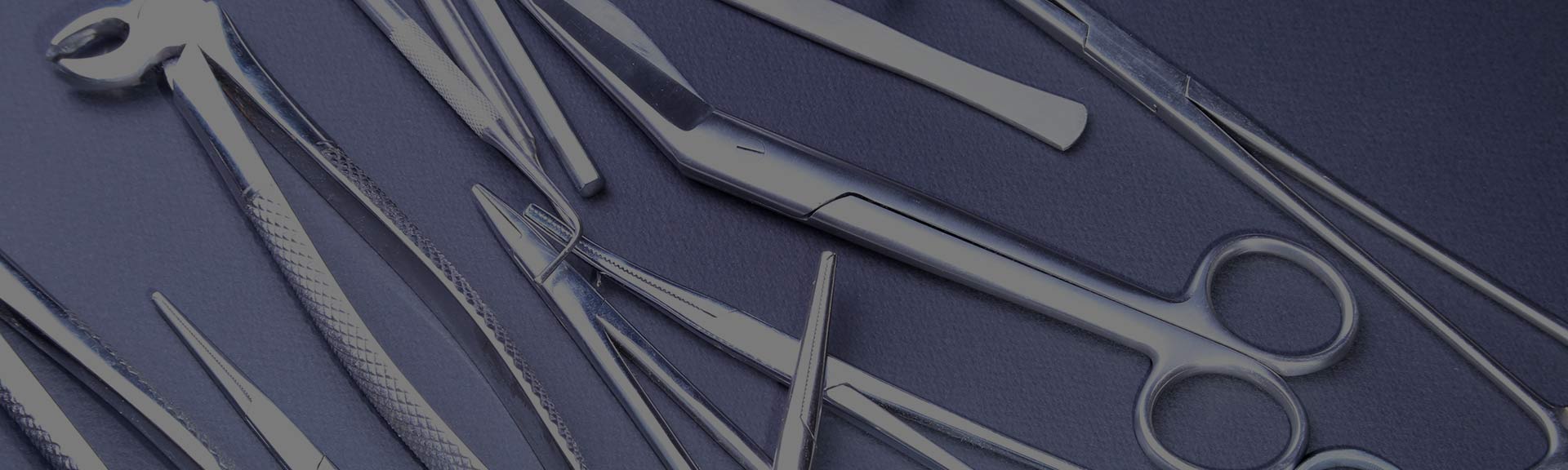
Improved cash flow for healthcare practices
By outsourcing medical billing, healthcare providers can see an improvement in their cash flow as claims are processed faster and with fewer errors.
Reduced administrative burden and costs
By outsourcing medical billing, healthcare providers can reduce the administrative burden on their staff and cut down on associated costs such as training, software, and office space.
Enhanced accuracy and compliance with regulations
Medical billing services are staffed with trained professionals who are knowledgeable about the latest regulations and compliance requirements. This can lead to increased accuracy and reduced errors in the billing process.
Cost savings
Outsourcing medical billing can save healthcare providers significant amounts of money on salaries, benefits, and overhead costs associated with hiring and managing an in-house billing staff.
Increased revenue
Professional medical billing services can often increase a healthcare practice’s revenue by submitting cleaner claims, reducing denials, and following up on unpaid claims in a timely manner.
Access to expert billing knowledge
Medical billing companies employ experts in the field who stay up-to-date with the latest industry changes, regulations, and best practices.
Reduced billing errors
Medical billing services use sophisticated software and systems to reduce errors and ensure that all claims are submitted correctly.
Improved cash flow
Outsourcing medical billing allows healthcare providers to focus on patient care, while the billing company handles the administrative tasks of submitting claims and following up on payments, leading to improved cash flow.
Efficient claims processing
Medical billing companies are equipped with specialized technology and skilled staff to process claims efficiently, reducing the time it takes for healthcare providers to receive payments.
Enhanced patient experience
When healthcare providers outsource their medical billing, their staff can focus on providing quality care to patients, rather than spending time on administrative tasks.
Scalability
Outsourcing medical billing services allow healthcare providers to easily scale their billing operations up or down as needed to accommodate changes in patient volume.
Reduced billing cycle time
With efficient claims processing and follow-up, outsourcing medical billing can reduce the time it takes for healthcare providers to receive payments, leading to faster revenue cycles.
Reduced administrative burden
Medical billing companies take care of all aspects of the billing process, from submitting claims to following up on denials, reducing the administrative burden on healthcare providers and their staff.
How to Choose a Medical Billing Service
Factors to consider include the experience of the service provider, the quality of their software, their reputation, and their pricing structure.
Questions to ask include inquiries about their experience with your specific type of healthcare practice, their approach to customer service, and how they handle potential issues or disputes.
Common Medical Billing Errors to Avoid
Incorrect patient information
Billing errors often occur when patient information is incorrect or incomplete. It’s important to verify all patient information, including name, address, date of birth, and insurance information, before submitting claims.
Coding errors
Medical billing codes are complex and constantly changing, which can lead to errors. Common coding errors include using outdated codes, applying the wrong code for a procedure, or using the wrong modifier.
Incomplete documentation
Incomplete documentation can lead to denied claims, delayed payments, or audits. It’s important to ensure that all necessary information is included in the medical record and that it supports the billing codes used.
Upcoding or unbundling
Upcoding is the practice of submitting claims for services or procedures that are more expensive than what was actually provided while unbundling is the practice of submitting separate claims for services that should be billed together.
Duplicate billing
Duplicate billing occurs when the same service or procedure is billed more than once, which can lead to claim denials and audits.
Incorrect insurance information
It’s important to verify insurance information before submitting claims, as errors can lead to claim denials or delays in payment.
Failure to follow up on denials
When a claim is denied, it’s important to determine the reason for the denial and take action to resolve it. Failure to follow up on denials can result in lost revenue and increased administrative costs.
Best practices for avoiding errors in medical billing
Best practices for avoiding errors include double-checking patient information, reviewing coding regularly, and staying up-to-date on changes in billing regulations.
How Medical Billing Services Help with Claims Processing
Overview of the claims process in medical billing
The claims process involves submitting medical billing information to insurance companies and following up on any issues or denials.
Medical billing services can improve claims processing by ensuring accurate coding and timely submission of claims. They can also follow up on claims denials and resubmit them with the appropriate documentation.
The Role of Technology in Medical Billing Services
Overview of the technological tools used in medical billing: Technological tools used in medical billing include software for claims processing, electronic health records (EHRs), and data analytics.
How technology can improve the efficiency and accuracy of medical billing services: Technology can improve the efficiency and accuracy of medical billing services by automating repetitive tasks, reducing errors, and providing real-time data on billing performance.
Understanding Medical Coding in Medical Billing
Overview of medical coding and its importance in medical billing
Medical coding is the process of translating medical procedures and diagnoses into standardized codes for billing purposes.
Medical billing services can provide training and support to healthcare providers on the latest coding systems and how to use them effectively.
How Medical Billing Services Help with Revenue Cycle Management
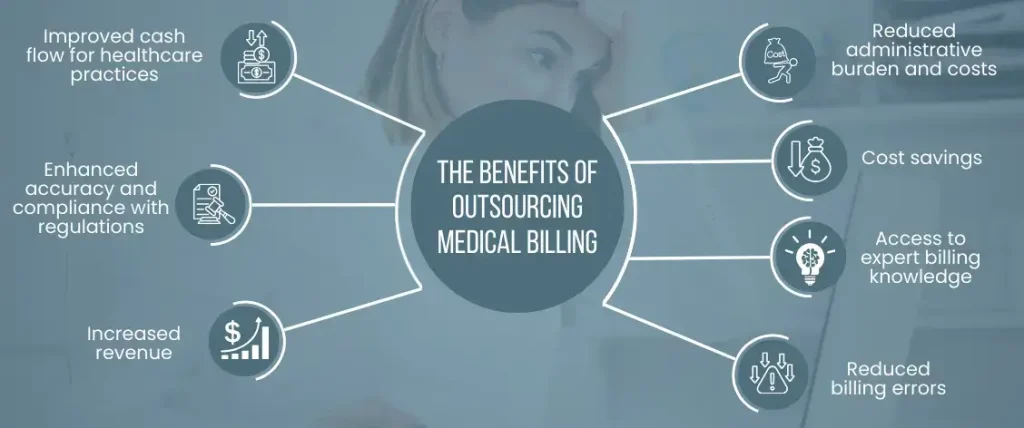
Overview of the revenue cycle in healthcare practices
The revenue cycle involves all aspects of the financial process in healthcare practice, from scheduling and registration to claims processing and collections.
Claims submission
Medical billing services have the expertise and technology to submit claims quickly and accurately, reducing the time it takes to receive payment and improving the revenue cycle.
Claim follow-up
Medical billing services can help healthcare providers follow up on unpaid claims, which can help to identify and resolve any issues causing payment delays.
Denial management
Medical billing services can help healthcare providers identify and resolve reasons for claim denials, such as incorrect coding or missing information, improving the likelihood of getting claims paid in full.
Payment posting
Medical billing services can post payments received from insurance companies, government payers, and patients, ensuring that payments are accurately applied to patient accounts.
Patient statements
Medical billing services can generate patient statements for outstanding balances and track patient payments, improving revenue cycle management.
Collections
Medical billing services can help healthcare providers collect unpaid balances by sending reminders, making phone calls, and setting up payment plans with patients.
Insurance verification
Medical billing services can verify insurance coverage for patients before services are provided, reducing the likelihood of denied claims and ensuring that patients receive the care they need.
Financial reporting
Medical billing services can provide healthcare providers with detailed financial reports that show trends in revenue, expenses, and profitability, allowing providers to make informed decisions about their practices.
Compliance monitoring
Medical billing services can help healthcare providers stay compliant with regulatory requirements, such as HIPAA and the Affordable Care Act, reducing the risk of audits and penalties.
Customized solutions
Medical billing services can offer customized solutions based on the unique needs of each healthcare provider, improving the efficiency and effectiveness of revenue cycle management.
Medical billing services can support revenue cycle management by streamlining the billing process and providing real-time data on billing performance, allowing healthcare providers to identify areas for improvement and increase their profits.
The Importance of HIPAA Compliance in Medical Billing
Overview of HIPAA regulations and their impact on medical billing, The Health Insurance Portability and Accountability Act (HIPAA) sets national standards for the protection of patient health information and affects all aspects of healthcare, including medical billing.
How medical billing services can ensure compliance with HIPAA regulations, Medical billing services can ensure compliance with HIPAA regulations by implementing the necessary safeguards and policies to protect patient health information, such as secure data storage and transmission, employee training, and risk assessments.
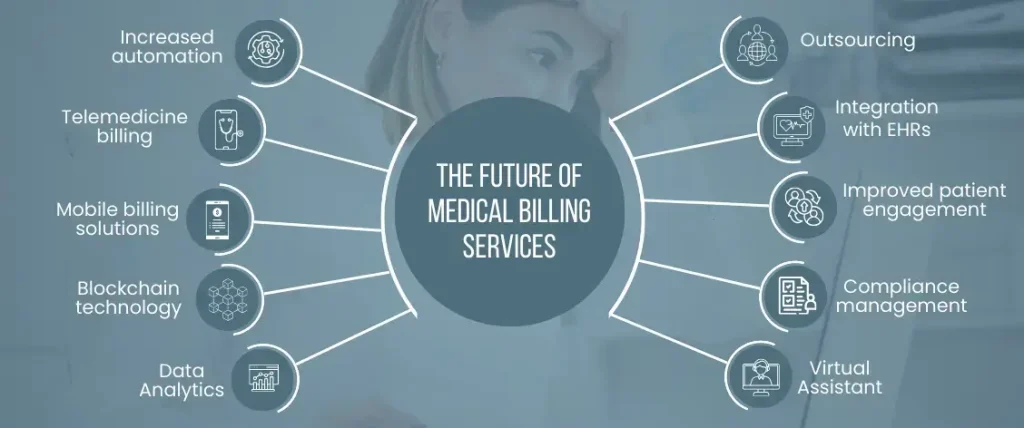
The Future of Medical Billing Services
Increased automation
Medical billing services are likely to become more automated in the future, with the use of machine learning and artificial intelligence to improve accuracy and efficiency.
Telemedicine billing
With the growth of telemedicine, medical billing services will need to adapt to new billing codes and reimbursement rules for virtual visits.
Mobile billing solutions
Medical billing services will increasingly be able to provide mobile billing solutions that enable providers to submit and track claims on the go.
Blockchain technology
The use of blockchain technology in medical billing could improve security, transparency, and accuracy in payment processing.
Data Analytics
Medical billing services will continue to use data analytics to identify trends and patterns in claims and payments, improving revenue cycle management.
Outsourcing
More healthcare providers are expected to outsource their medical billing to third-party providers, allowing them to focus on patient care and reduce administrative burdens.
Integration with EHRs
Medical billing services will increasingly integrate with electronic health records (EHRs) to streamline the billing process and reduce errors.
Improved patient engagement
Medical billing services will focus on improving patient engagement in the billing process, with the use of patient portals and other tools to provide transparency and convenience.
Compliance management
Medical billing services will continue to evolve to meet changing regulatory requirements, including those related to privacy and security.
Virtual Assistant
Medical billing services will leverage virtual assistants and chatbots to improve customer service and support, providing patients and providers with quick access to billing information and support.
How these technologies are expected to impact medical billing services in the future:
Artificial intelligence
The use of artificial intelligence (AI) in medical billing services is expected to increase accuracy and efficiency, with AI algorithms able to identify coding errors and automatically submit claims.
Blockchain technology
Blockchain technology is expected to improve security and transparency in the medical billing process, with blockchain-enabled payment systems reducing the risk of fraud and ensuring prompt payment.
Data analytics
The use of data analytics in medical billing services is expected to improve revenue cycle management, with analytics tools providing insights into claim trends and payment patterns that can inform billing strategies.
Telemedicine
The growth of telemedicine is expected to drive the development of new billing codes and reimbursement rules for virtual visits, with medical billing services adapting to these changes.
Mobile technology
The use of mobile technology in medical billing services is expected to increase, with mobile billing solutions allowing providers to submit and track claims on-the-go, and patients able to use mobile apps to view their bills and make payments.
Choosing Between In-House and Outsourced Medical Billing
Pros and cons of in-house medical billing
In-house medical billing can provide greater control and visibility over the billing process, but it can also be expensive and time-consuming.
Outsourcing medical billing can provide cost savings and improve efficiency, but it can also result in less control over the billing process and potentially lower quality service.
Factors to consider when choosing between in-house and outsourced medical billing: Factors to consider include the size and complexity of the healthcare practice, the experience and expertise of the staff, and the available resources.
How to Evaluate the Success of Medical Billing Services
Clean claim rate
The clean claim rate measures the percentage of claims that are paid without any errors or rejections. A high clean claim rate is an indicator of a successful medical billing service, as it demonstrates accuracy in coding and billing.
Days in accounts receivable
This metric measures the average number of days it takes to receive payment for services rendered. A low number of days in accounts receivable indicates that claims are being processed quickly and efficiently, leading to better cash flow.
Denial rate
The denial rate measures the percentage of claims that are denied by insurance companies or other payers. A low denial rate is an indicator of a successful medical billing service, as it suggests that claims are being submitted correctly and with complete information.
Patient collections
The patient collections rate measures the percentage of patient balances that are collected by the medical billing service. A high patient collections rate indicates that the medical billing service is effective in collecting patient balances, improving the overall revenue cycle.
Provider reimbursement
The provider reimbursement rate measures the percentage of expected reimbursement that is actually received. A high provider reimbursement rate is an indicator of a successful medical billing service, as it suggests that claims are being paid in full and in a timely manner.
Customer satisfaction
Customer satisfaction measures the level of satisfaction of healthcare providers with the medical billing service. A high customer satisfaction rate indicates that the medical billing service is meeting the needs of healthcare providers and delivering high-quality services.
Accuracy of coding
The accuracy of coding measures the percentage of codes that are correctly applied to services rendered. A high accuracy of coding rate indicates that the medical billing service is applying the correct codes, reducing the risk of claim denials or delays.
Claims follow-up
The claims follow-up rate measures the percentage of claims that are followed up on after initial submission. A high claims follow-up rate indicates that the medical billing service is proactive in resolving issues with denied or delayed claims.
Compliance with regulations
Compliance with regulations measures the extent to which the medical billing service adheres to regulatory requirements, such as HIPAA and the Affordable Care Act. A high compliance rate indicates that the medical billing service is protecting patient privacy and meeting legal requirements.
Return on investment (ROI)
The ROI measures the financial return on the investment in medical billing services. A high ROI indicates that the medical billing service is delivering value to healthcare providers and contributing to the overall financial success of the practice.
By analyzing these metrics, healthcare providers can identify areas for improvement in their billing process and work with their medical billing service provider to address any issues and maximize revenue.
How Medmax is Changing the Landscape
Medical billing services play a critical role in the healthcare industry, allowing medical professionals to focus on their core responsibilities while leaving the billing and administrative tasks to experts. Medmax medical billing company stands out in the industry for its dedication to providing exceptional services to our clients. With years of experience and a team of skilled professionals, we have established ourselves as a trusted partner for medical practices seeking to streamline their billing process, reduce costs, and increase revenue. We are committed to accuracy, efficiency, and customer satisfaction sets us apart from our competitors, making us an ideal choice for any medical practice looking for reliable and effective medical billing services.