Denial Management Services: A Step-by-Step Guide for Providers
Table of Contents
ToggleDenial Management Services
Denial management services are an essential aspect of healthcare that requires organizations to effectively handle and process insurance claims. With the ever-evolving healthcare industry, it has become increasingly challenging for healthcare providers to manage the high volume of insurance claims, track the status of claims, and appeal denials in a timely manner. As a result, denial management services have become a critical function that requires a well-coordinated effort between healthcare providers, insurance companies, and patients.
Understanding Denials in Healthcare
Denials in healthcare refer to the rejection of payment for a medical service or procedure by a patient’s insurance company. They can occur for a variety of reasons, including lack of prior authorization, incorrect coding, or failure to meet medical necessity criteria. Understanding the reasons behind denials and the denial management services for appealing them is crucial for healthcare providers looking to maximize revenue and protect their financial stability.
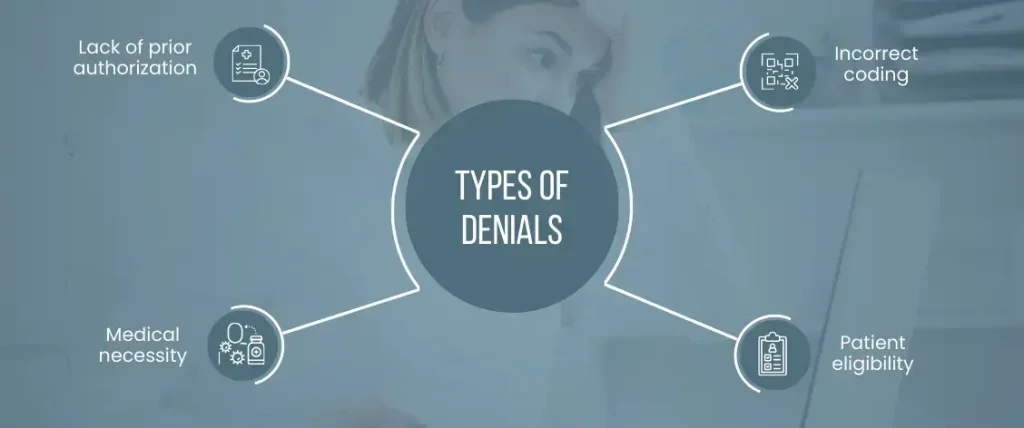
Types of Denials
There are several types of denials that healthcare providers may encounter, including:
Lack of prior authorization
If a service or procedure requires prior authorization from the insurance company, and the authorization is not obtained, the claim may be denied.
Incorrect coding
Healthcare providers must use specific codes to describe the services they provide. If the codes are incorrect or outdated, the claim may be denied.
Medical necessity
Insurance companies may deny a claim if they determine that a service or procedure was not medically necessary. This may occur if the insurance company feels that the service was not essential for the patient’s health or well-being.
Patient eligibility
If a patient is not eligible for coverage under their insurance plan, their claims may be denied.
Appealing Denials
When a claim is denied, healthcare providers have the option to appeal the decision. The appeal process typically involves the submission of additional documentation and a written explanation of why the service or procedure was necessary. The insurance company will review the appeal and make a final determination. If the appeal is denied, healthcare providers may have the option to appeal again, although the outcome of subsequent appeals may be uncertain.
The Impact of Denials on Healthcare Organizations
The impact of denials on healthcare organizations can be far-reaching and significant. When a claim is denied, it means that the healthcare provider must either bill the patient directly for the service or write off the cost as uncollectable. This can result in lost revenue, increased administrative costs, and decreased profitability for the healthcare organization.
Lost Revenue
When a claim is denied, it means that the healthcare provider is not receiving payment for the service provided. This can result in a significant loss of revenue for the organization, especially if the denial is for a high-cost service. This lost revenue can have a direct impact on the financial stability of the healthcare organization.
Increased Administrative Costs
The denial management services appealing a denied claim can be time-consuming and complex. It requires the healthcare provider to gather supporting documentation, prepare a well-written appeal letter, and respond promptly to any requests for additional information from the insurance company. This process can be both time-consuming and costly, requiring dedicated staff and resources.
Decreased Profitability
When denials are not effectively managed, they can result in decreased profitability for the healthcare organization. The increased administrative costs associated with appeals and the loss of revenue from denied claims can have a significant impact on the bottom line. Additionally, if the denial management services is not streamlined and efficient, it can result in decreased productivity and increased expenses for the healthcare organization.
Denials can also have a negative impact on patient satisfaction and loyalty. If a patient is billed directly for a service that was initially submitted to the insurance company, they may feel frustrated and misled. This can result in a loss of trust in the healthcare provider, and the patient may choose to seek care elsewhere in the future.
Denials can have a significant impact on healthcare organizations. From lost revenue and increased administrative costs to decreased profitability and decreased patient satisfaction, it is essential for healthcare providers to have a comprehensive denial management strategy in place to effectively manage denials and protect their financial stability.
Doctor touching medical icon network connection on laptop and tablet with modern virtual screen interface, medical technology network concept
Strategies for Effective Management
To effectively manage denials, healthcare providers must have a comprehensive strategy in place. Some strategies that have proven effective in managing denials include:
- Implementing a proactive denial management services.
- Conducting regular claims audits to identify trends and root causes of denials.
- Providing staff with ongoing education and training on insurance regulations and coding practices.
- Establishing a dedicated team.
- Utilizing technology to streamline the process and increase efficiency.
The Role of Technology in Denial Management
Technology has revolutionized the healthcare industry, and Denial management is no exception. Today, healthcare organizations can utilize various technologies to automate and streamline the process. For example, providers can use software to track claims, receive notifications of denied claims, and automate the appeals process. This technology can help providers respond to denials more quickly, reduce administrative costs, and increase the chances of a successful appeal.
Tips for Successful Appeal Process
If a claim is denied, healthcare providers can appeal the decision to the insurance company. The appeal process can be time-consuming and complex, but a successful appeal can result in payment for the denied claim. Some tips for a successful appeal process include:
- Review the denial reason and gather supporting documentation.
- Prepare a well-written and persuasive appeal letter.
- Respond promptly to requests for additional information from the insurance company.
- Utilize technology to track the status of the appeal and receive notifications of any updates.
Wrap Up!
It is a critical function in healthcare that requires a well-coordinated effort between healthcare providers, insurance companies, and patients. By understanding the impact of denials, implementing a comprehensive denial management strategy, utilizing technology, and following best practices for the appeal process, healthcare providers can effectively manage denials and maintain their financial stability. However, with the help of a specialized medical billing company like Medmax, healthcare providers can focus on providing high-quality patient care while leaving the management of insurance claims and appeals in the hands of experts.
How Medmax Can Help?
Medmax has a team of highly skilled professionals who have extensive knowledge of the healthcare industry and insurance regulations. They use cutting-edge technology to streamline the process, increasing efficiency and reducing administrative costs. Additionally, Medmax provides ongoing education and training to healthcare providers, ensuring that they stay up-to-date on the latest industry trends and regulations.
Outsourcing denial management services to Medmax can provide healthcare providers with peace of mind, knowing that their insurance claims and appeals are being handled by experts. With a successful track record of managing denials and maximizing revenue, healthcare providers can rest assured that their financial stability will be protected.
In today’s fast-paced and ever-evolving healthcare industry, outsourcing denial management to Medmax can be a smart business decision. By freeing up time and resources, healthcare providers can focus on providing high-quality patient care, and leave the management of insurance claims and appeals to the experts at Medmax.

Emily Thompson
Emily Thompson is a Revenue Cycle Management (RCM) Specialist with extensive experience in the medical billing industry. She helps healthcare organizations and medical billing companies improve claim efficiency, reduce A/R backlogs, and implement data-driven RCM strategies. Emily’s articles focus on end-to-end medical billing services, denial prevention, and technology-driven revenue optimization for healthcare practices across the U.S.