Maximizing Reimbursement: Medical Billing and Coding Guide
Table of Contents
ToggleIntroduction to Medical Billing and Coding
Definition and Overview
Medical billing is the process of submitting and following up on claims to insurance companies and patients for payment for medical services. Medical coding, on the other hand, involves the use of codes to classify medical diagnoses and procedures for reimbursement purposes. Both medical billing and coding are critical components of the healthcare industry as they ensure that patients receive the proper medical treatment and healthcare providers receive payment for their services.
Importance in the Healthcare Industry
Medical billing and coding play a critical role in the healthcare industry by ensuring that medical claims are processed accurately and efficiently. This helps to reduce costs, improve patient outcomes, and ensure that healthcare providers receive reimbursement for their services. Accurate medical billing and coding also help to reduce fraud and abuse in the healthcare system, which can have a significant impact on the overall cost of healthcare.
Career Opportunities in Medical Billing and Coding
The demand for skilled medical billers and coders is on the rise, and there are many career opportunities for those interested in this field. Medical billing and coding professionals may work in a variety of settings, including hospitals, medical offices, and insurance companies. They may also work as remote medical billers and coders, which is a flexible and convenient option for many individuals. The demand for skilled medical billers and coders is expected to grow in the coming years, making it an excellent career choice for those seeking a stable and growing field.
Required Skills and Qualifications
To be successful in a career in medical billing and coding, individuals must possess a strong understanding of medical terminology, anatomy, and physiology. They must also be detail-oriented and have excellent organizational skills. In addition, medical billers and coders must be able to work well under pressure and meet deadlines. A certification in medical billing and coding is typically required for entry-level positions, and ongoing education and training are important to maintain professional competency and stay current with changes in the field.
Education and Training Requirements
To become a medical biller or coder, individuals typically need to complete a certificate program in medical billing and coding. These programs typically cover medical terminology, anatomy and physiology, medical billing and coding processes, and reimbursement methodologies. Associate’s and bachelor’s degree programs in healthcare management or a related field are also available for those who want to pursue a more advanced education. In addition to formal education, ongoing professional development and continuing education are critical for medical billing and coding professionals to maintain their knowledge and skills in a rapidly changing field.
Certification Options
Certification in medical billing and coding demonstrates a level of expertise and professionalism in the field. There are several certifying organizations that offer certifications in medical billing and coding, including the American Academy of Professional Coders (AAPC), the American Health Information Management Association (AHIMA), and the National Healthcare Association (NHA). Each organization has its own certification requirements, and it is important to research the options to determine which certification is the best fit for an individual’s career goals and professional development needs.
Benefits of Certification
Certification in medical billing and coding has many benefits, including increased job opportunities, higher salaries, and improved professional credibility. Certified medical billers and coders are in high demand, and many employers prefer to hire certified professionals for their expertise and knowledge in the field. Certification also demonstrates a commitment to professional development and ongoing learning, which can be a valuable asset in the competitive job market.
Medical billing and coding are essential components of the healthcare industry that ensure that patients receive the proper medical treatment and healthcare providers receive reimbursement for the services they provide. This field offers exciting career opportunities for those interested in pursuing a career in healthcare, and certification can be a valuable asset for those looking to advance their careers and increase their earning potential. Whether an individual is just starting their career or looking to make a change, a career in medical billing and coding can be a rewarding and fulfilling choice.
Types of Medical Billing and Coding Systems
There are several types of billing and coding systems available, each with its own set of features and benefits. Understanding the different types of systems can help healthcare providers choose the best solution for their needs. This section will provide an overview of the most common types of medical billing systems.
Manual Systems
Manual medical systems involve manual data entry and record-keeping. This type of system is often used by smaller healthcare providers who have a limited number of patients and a smaller volume of claims. Manual systems are simple to use, but they can be time-consuming and prone to errors, which can result in denied claims and delayed payments
Electronic Medical Records (EMR) Systems
Electronic Medical Records (EMR) systems are a type of billing and coding system that allows healthcare providers to store, manage, and access patient information electronically. EMR systems provide real-time access to patient information, allowing healthcare providers to make informed decisions and provide better care. EMR systems are more efficient and accurate than manual systems, but they can be more complex and require a higher level of technical expertise.
Integrated Systems
Integrated systems are a combination of manual and electronic medical coding systems. They allow healthcare providers to take advantage of the benefits of both manual and electronic systems, providing an efficient and effective solution for their needs. Integrated systems are typically used by larger healthcare providers who have a high volume of claims and need a more sophisticated solution for their medical billing and coding needs.
Web-Based Systems
Web-based billing systems are designed to be accessed via the internet. This type of system is ideal for healthcare providers who want to access their medical billing information from any location with an internet connection. Web-based systems are typically more cost-effective than traditional systems, but they may be subject to security and reliability issues.
Cloud-Based Systems
Cloud-based coding systems are a type of web-based system that provides secure, remote access to medical coding information. Cloud-based systems are ideal for healthcare providers who need to access their medical billing and coding information from multiple locations or who want to reduce their IT costs. Cloud-based systems offer enhanced security, scalability, and reliability, making them an excellent choice for healthcare providers of all sizes.
Factors to Consider When Choosing a Medical Billing and Coding System
Choosing the right system is an important decision that can have a significant impact on a healthcare provider’s efficiency, accuracy, and profitability. This section will provide an overview of the factors that healthcare providers should consider when choosing a billing and coding system.
Budget
The cost of a system is an important factor to consider when choosing a solution. Healthcare providers should consider their budget and the total cost of ownership when making their decision, including the cost of hardware, software, installation, and training.
Ease of Use
The ease of use of a medical coding system is also an important factor to consider. Healthcare providers should choose a solution that is intuitive and easy to use, to ensure that their staff can work efficiently and accurately.
Functionality
The functionality of a coding system is also critical. Healthcare providers should choose a solution that provides the features and capabilities they need to manage their medical billing needs effectively.
Integration
Integration with other systems and applications is an important factor to consider when choosing a system. Healthcare providers should choose a solution that integrates seamlessly with their existing systems and processes, to ensure a smooth and efficient workflow.
Security
The security of information is critical, as it contains sensitive patient information. Healthcare providers should choose a solution that offers strong security measures, such as encryption, access control, and audit trails, to protect their patient information from theft and misuse.
Training and Support
Training and support are also important factors to consider when choosing a system. Healthcare providers should choose a solution that provides comprehensive training and support, to ensure that their staff can use the system effectively and resolve any issues that may arise.
Scalability
Scalability is an important factor to consider when choosing a medical coding system. Healthcare providers should choose a solution that can scale to meet their growing needs, as their patient volume and complexity increase.
Compatibility
Compatibility with other systems and applications is also an important factor to consider when selecting a billing system. Healthcare providers should choose a solution that is compatible with their existing systems and processes, to ensure a seamless integration.
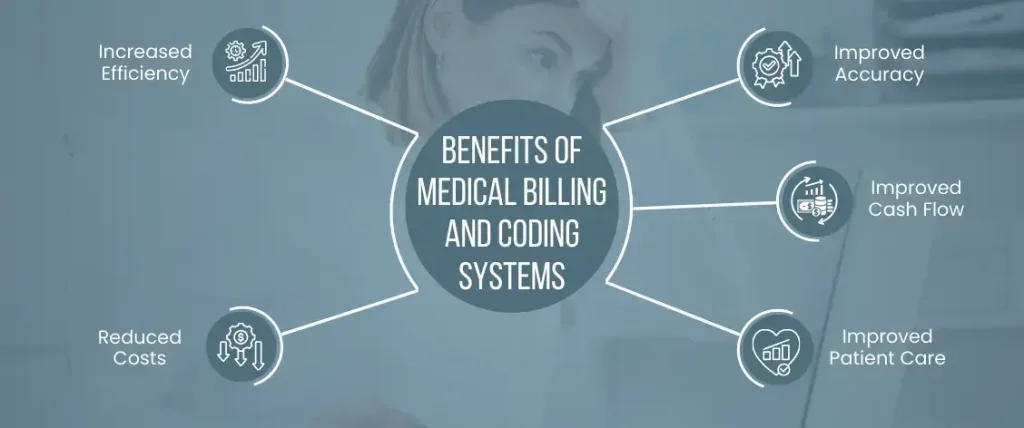
Benefits of Medical Billing and Coding Systems
Medical billing systems offer a number of benefits to healthcare providers, including increased efficiency, accuracy, and profitability. This section will provide an overview of the key benefits of medical systems.
Increased Efficiency
Systems can increase efficiency by automating many manual tasks, reducing the time required to process claims and increasing the accuracy of the information processed.
Improved Accuracy
Systems can improve accuracy by reducing the number of errors that occur during manual data entry, providing real-time access to patient information, and reducing the risk of denied claims.
Reduced Costs
Systems can reduce costs by automating many manual tasks, reducing the time required to process claims, and reducing the risk of denied claims.
Improved Cash Flow
Systems can improve cash flow by reducing the time required to process claims, improving the accuracy of the information processed, and reducing the risk of denied claims.
Improved Patient Care
Systems can improve patient care by providing real-time access to patient information, allowing healthcare providers to make informed decisions and provide better care.
Medical coding systems are an essential tool for healthcare providers, providing increased efficiency, accuracy, and profitability. Understanding the different types of systems available, the factors to consider when choosing a solution, and the benefits of medical billing and coding systems is critical for healthcare providers to make informed decisions about their medical billing and coding needs.