Understanding the Medical Billing Process Steps
Table of Contents
ToggleDefinition and Purpose of Medical Billing
Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for medical services rendered. It is an important part of the healthcare industry as it ensures healthcare providers are properly compensated for their services. Accurate and timely medical billing is critical to ensure claims are paid correctly and on time.
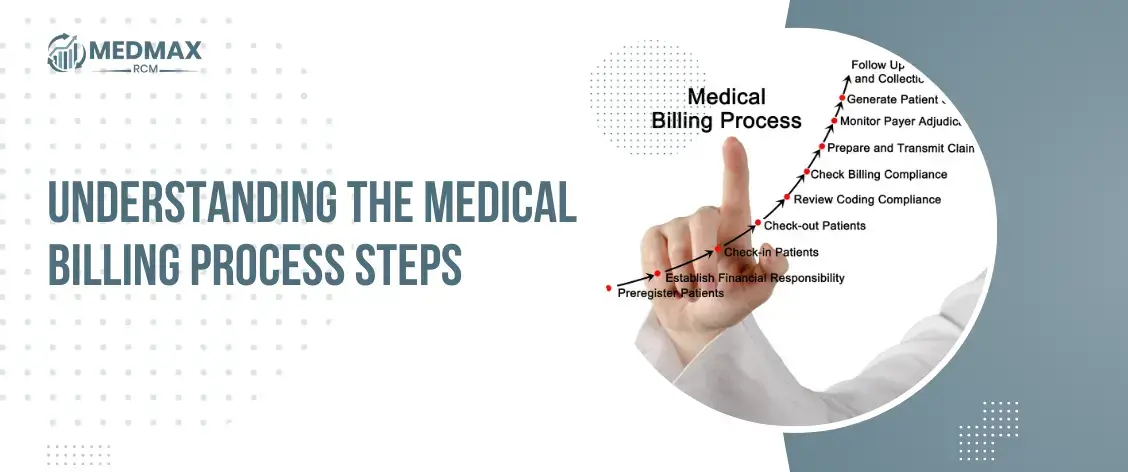
Key Components of the Medical Billing Process Steps
There are several key components involved in the medical billing process, including patient registration, insurance verification, coding and documentation, claim creation and submission, payment posting, and follow-up. Patient registration and insurance verification are necessary to collect and verify patient information and insurance eligibility. Coding and documentation involve the process of assigning codes to medical procedures and diagnoses to ensure accurate billing. Claim creation and submission involve the creation of a claim form and submission to the insurance company for payment. Payment posting and follow-up are the final steps in the medical billing process steps, which involve posting payments and following up on denied or unpaid claims.
The Importance of Accurate and Timely Medical Billing
It is essential to have medical billing that is both accurate and timely in order to guarantee that claims will be paid appropriately and on time. Incorrect medical billing can result in claims being denied, payments being delayed, and even legal complications. In order to guarantee precise and timely medical billing, it is essential to be current on the many legislation and procedures that are subject to change.
Preparing for Medical Billing
Patient Registration and Insurance Verification: Patient registration involves collecting and verifying patient demographic information, such as name, address, and insurance information. Insurance verification is the process of verifying the patient’s insurance coverage and eligibility for medical services plus provider credentialing. This step is important to ensure that the healthcare provider is authorized to provide medical services and to avoid claim denials.
Establishing and Updating Patient Records
Accurate and up-to-date patient records are essential for proper medical billing. These records include medical history, allergies, and medication lists, and are used to support the coding and medical billing process steps. It is important to maintain confidentiality and comply with HIPAA regulations to protect patient privacy.
Ensuring HIPAA Compliance
HIPAA regulations are a set of federal guidelines designed to protect the privacy and security of patient health information. It is essential to comply with HIPAA regulations when preparing for medical billing. This includes protecting patient information, obtaining proper authorization for the release of medical records, and ensuring that all employees are properly trained in HIPAA compliance.
Creating and Submitting Claims
Coding and Documentation
Claim Creation and Validation
Once the claim form is complete, it must be validated for accuracy and completeness before submission. This includes ensuring that all required fields are complete, that the coding is accurate, and that the claim is formatted correctly. A validated claim is more likely to be paid on time and in full by the insurance company.
Electronic vs. Paper Claims
Electronic claims submission is becoming more common in the medical billing industry due to its efficiency and speed. Electronic claims are submitted electronically through a clearinghouse, which can save time and reduce errors. Paper claims are still used in some situations, such as when electronic submission is not possible or the healthcare provider prefers to submit claims by mail.
Payment Posting and Follow-up
Payment Posting and Reconciliation
Once a claim has been paid, the payment must be recorded and posted to the patient’s account. Payment posting involves verifying that the payment matches the expected amount, reconciling any differences, and updating the patient’s account accordingly. Accurate payment posting is important for maintaining financial records and ensuring that patients are billed correctly for any remaining balances.
Denial Management
Denials occur when an insurance company refuses to pay all or part of a claim. Denial management involves identifying the reason for the denial, correcting any errors or omissions, and resubmitting the claim for payment. It is important to track and monitor denials to identify patterns and areas for improvement in the medical billing process steps.
Appeals Process
If a claim is denied and resubmission is unsuccessful, an appeal can be filed with the insurance company. The appeals process involves providing additional documentation or supporting evidence to support the claim and contest the denial. This process can be time-consuming but is often necessary to ensure that healthcare providers receive appropriate payment for services rendered.
Compliance and Quality Assurance
Compliance with Regulations
Medical billing is subject to numerous regulations and guidelines at the federal, state, and local levels. These regulations include HIPAA, Medicare, and Medicaid guidelines, as well as regulations related to coding and documentation. Compliance with these regulations is essential to avoid legal issues and to maintain patient trust and confidence.
Quality Assurance
Quality assurance involves monitoring and evaluating the medical billing process steps to ensure that it is effective and efficient. This includes tracking metrics such as claim acceptance rates, payment turnaround times, and denial rates. Quality assurance can help identify areas for improvement in the medical billing process steps and improve overall performance.
In summary, the medical billing process steps are complex and important parts of the healthcare industry. Understanding the key components of the process and preparing for accurate and timely billing is essential to ensure that healthcare providers receive appropriate payment for services rendered. Creating and submitting accurate claims, and managing payments and denials are important for maintaining financial records and ensuring patient satisfaction. Compliance with regulations and quality assurance measures helps to ensure that the medical billing process steps is effective and efficient.

Related Posts
Emily Thompson
Emily Thompson is a Revenue Cycle Management (RCM) Specialist with extensive experience in the medical billing industry. She helps healthcare organizations and medical billing companies improve claim efficiency, reduce A/R backlogs, and implement data-driven RCM strategies. Emily’s articles focus on end-to-end medical billing services, denial prevention, and technology-driven revenue optimization for healthcare practices across the U.S.