99213 CPT Code: Wound Care Billing Explained
CPT Code 99213 is an Evaluation & Management (E/M) code for an established patient’s office/outpatient visit, often used in wound care for follow-up visits involving low-complexity medical decision-making (MDM) or 20-29 minutes of total encounter time, covering things like routine wound checks, minor adjustments, or stable chronic wound management, requiring history, exam, and care coordination. It’s for less complex care than 99214 (moderate complexity) but more than 99212 (routine check).
As a wound care professional, CPT codes are a routine part of your daily workflow. One of the most frequently used codes in outpatient wound care is the 99213 CPT code, which applies to established patient visits. Because wound treatment often involves ongoing follow-ups, providers regularly face decisions about whether 99213 is appropriate or if a higher or lower E/M code should be reported. Understanding how 99213 fits within the broader E/M code range is essential for accurate billing and compliance.
This guide explains what CPT codes are, why correct coding matters, and how the 99213 CPT code is used in wound care. It also highlights documentation requirements, common coding challenges, and key differences between 99212, 99213, and 99214 to help you code with confidence.
Table of Contents
ToggleWhat Are CPT Codes?
Current Procedural Terminology (CPT) codes are a standardized medical coding system created and maintained by the American Medical Association (AMA). These five-digit numeric codes describe medical, diagnostic, and surgical services, ranging from routine office visits to complex procedures.
CPT codes are updated annually to reflect changes in medical practice, technology, and clinical standards. They are widely used by physicians, hospitals, outpatient clinics, and other healthcare organizations across the United States.
CPT codes support healthcare operations in several important ways:
- Clear communication: CPT codes provide a common language that allows providers, payers, and healthcare organizations to clearly understand what services were performed.
- Billing and reimbursement: Accurate CPT coding ensures consistent claims submission and appropriate reimbursement from private insurers, Medicare, and Medicaid.
- Data tracking and analysis: CPT data is used to monitor healthcare utilization, analyze treatment trends, and support clinical research.
Why Accurate Coding Matters in Wound Care
Proper CPT coding is far more than a billing requirement it directly impacts the success and sustainability of a wound care practice.
Accurate coding helps ensure:
- Appropriate reimbursement: Providers are paid fairly for the level of care delivered.
- Financial stability: Correct coding supports predictable cash flow and long-term practice viability.
- Regulatory compliance: Following CPT guidelines reduces the risk of audits, penalties, and payer disputes.
- Legal and ethical integrity: Accurate reporting is both a professional responsibility and a legal obligation.
- Improved patient care: Reliable coding data supports outcome tracking, quality improvement initiatives, and evidence-based care.
- Public health insights: Coding data helps identify trends in wound types and treatment outcomes, informing broader public health planning.
- Fewer claim denials: Clean, accurate claims reduce rework, administrative burden, and payment delays.
In short, effective coding is foundational to compliance, reimbursement, and high-quality patient care.
99213 CPT Code Explained
What Is the 99213 CPT Code?
CPT code 99213 describes an established patient office or outpatient visit requiring 20–29 minutes of total provider time on the date of service.
According to the AMA, 99213 applies to visits involving a stable chronic condition or an acute, uncomplicated injury. These encounters typically involve a low to moderate level of medical decision-making.
A 99213 visit generally includes:
- A medically appropriate history and/or physical examination
- Low-complexity medical decision-making
- Review of a limited amount of clinical data
- Low risk of complications or morbidity
This code is commonly reported by:
- Physicians (MDs and DOs)
- Nurse practitioners (NPs)
- Physician assistants (PAs)
Any qualified healthcare professional may bill 99213, provided the encounter meets the required criteria and aligns with state scope-of-practice regulations.
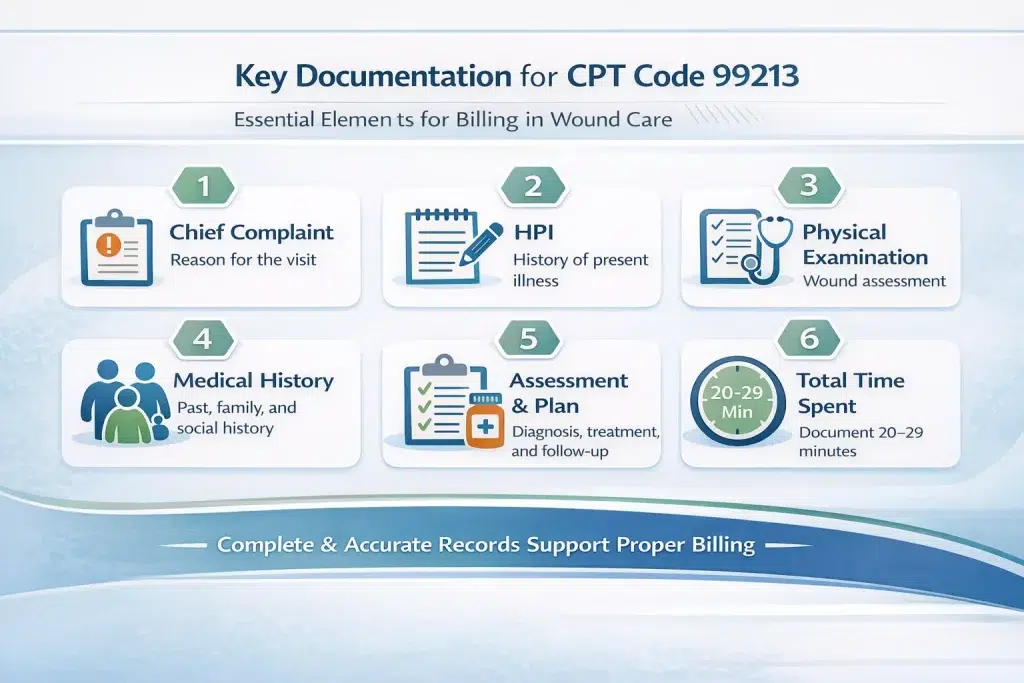
Documentation Requirements for CPT 99213
Thorough and accurate documentation is essential to support the use of CPT code 99213. Medical records should clearly reflect the services provided and justify the level of care billed.
Key documentation elements include:
- Chief complaint: The primary reason for the visit
- History of present illness (HPI): Including onset, duration, location, severity, and modifying factors
- Review of systems (ROS): Relevant systems reviewed based on the presenting problem
- Past, family, and social history: As applicable to the patient’s condition
- Physical examination: Problem-focused or expanded problem-focused exam relevant to wound care
- Assessment and plan: Diagnoses, treatment decisions, medications, tests, patient education, and follow-up
- Total time spent: Documentation of 20–29 minutes when billing based on time
Clear, concise, and complete documentation helps support claims and reduces audit risk.
Common Coding Challenges With 99213
Even experienced providers can encounter coding challenges. Common issues include:
- Upcoding: Billing a higher-level service than supported by documentation, which can result in audits, penalties, or payer sanctions
- Downcoding: Billing a lower-level service when a higher code is justified, leading to lost revenue
- Insufficient documentation: Missing details related to time, MDM, or clinical decision-making
- Misunderstanding guidelines: Incorrect application of E/M criteria for time, complexity, or data review
- Lack of ongoing education: Failure to stay current with CPT and CMS updates increases compliance risk
Avoiding these errors requires consistent documentation practices and regular coding education.
CPT 99212 vs 99213 vs 99214: Key Differences
CPT codes 99212, 99213, and 99214 are all used for established patient office visits, but they represent different levels of complexity, time, and medical decision-making.
CPT 99212
- Description: Self-limited or minor problem
- MDM: Straightforward to low complexity
- Time: 10–19 minutes
CPT 99213
- Description: Stable chronic condition or acute uncomplicated injury
- MDM: Low to moderate complexity
- Time: 20–29 minutes
CPT 99214
- Description: Worsening condition or problem requiring active medical management
- MDM: Moderate complexity
- Time: 30–39 minutes
| Aspect | 99212 | 99213 | 99214 |
|---|---|---|---|
| Complexity | Low | Low–Moderate | Moderate |
| Time | 10–19 min | 20–29 min | 30–39 min |
| History | Problem-focused | Expanded problem-focused | Detailed |
| Examination | Problem-focused | Expanded problem-focused | Detailed |
| Medical Decision-Making | Straightforward–Low | Low–Moderate | Moderate |
Tips for Accurate Use of CPT 99213
To ensure correct reporting of the 99213 CPT code:
- Understand the official E/M criteria
- Document time, MDM, history, and examination clearly
- Stay current with CPT and CMS updates
- Use trusted coding resources and expert guidance
- Perform regular internal chart audits
- Implement a formal coding compliance program with ongoing staff training
Why Accuracy Matters
Accurate coding for established patient visits like CPT 99213 supports fair reimbursement, regulatory compliance, and reliable clinical data. By applying the correct criteria, maintaining strong documentation habits, and staying informed on guideline changes, wound care providers can reduce errors, protect revenue, and deliver high-quality patient care.
Mastering CPT 99213 is not just about billing it’s about building a compliant, efficient, and patient-focused wound care practice. 99213 vs 99214 compares established patient visits where 99213 covers stable wounds (20–29 min) and 99214 covers more complex or worsening wounds (30–39 min).
Frequently Asked Question (FAQs)
What is the 99212 CPT code?
CPT code 99212 is for an Office/Outpatient Visit for an Established Patient with straightforward medical decision-making, typically involving 10-19 minutes of total time, and addressing a self-limited or minor problem. It’s the lowest-level evaluation and management (E/M) code for returning patients, used for routine follow-ups, medication adjustments for stable conditions, or simple health concerns.
What is the 99213 CPT code?
CPT code 99213 describes an office or outpatient visit for an established patient, involving a moderate level of complexity for evaluation and management (E/M) services, typically lasting 20-29 minutes, often for stable chronic conditions or minor new problems, requiring at least two of three components: history, exam, and low-complexity medical decision-making (MDM).
What is the 99214 CPT code?
CPT code 99214 describes an office or outpatient visit for an established patient, requiring a medically appropriate history/exam and a moderate level of medical decision-making (MDM), often taking 30-39 minutes of total time, used for managing more complex or chronic conditions.
What is CPT code 99213 used for?
CPT code 99213 is for an established patient’s office visit that involves a low-complexity level of medical decision-making or a total time of 20-29 minutes, used for routine follow-ups for stable chronic conditions (like managed hypertension) or minor acute issues (like a simple infection).
What services does CPT code 99213 cover?
CPT code 99213: Established patient office or other outpatient visit, 20-29 minutes. As the authority on the CPT code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care.
When to use 59 or 51 modifier?
Use Modifier 51 for multiple surgical procedures in the same session (telling payers which is primary vs. secondary for payment reduction) and Modifier 59 (Distinct Procedural Service) to override National Correct Coding Initiative (NCCI) edits when two bundled services were actually separate (e.g., different sites, encounters, incisions). Modifier 59 is the “modifier of last resort,” used to signal a legitimate exception to bundling rules, while 51 manages payment sequencing for typically related services.
What is the 99213 CPT code used for in wound care?
CPT code 99213 in wound care is for an Evaluation & Management (E/M) visit for an established patient with a stable chronic illness or uncomplicated injury, requiring low complexity medical decision-making, such as routine follow-up, medication management, or adjusting a treatment plan, often involving around 20-29 minutes of face-to-face time.
When should wound care providers use 99213 vs 99214?
Wound care providers use 99213 for low complexity visits (20-29 mins, stable issues, minimal data/risk) and 99214 for moderate complexity visits (30-39 mins, multiple or complex issues, moderate data/risk), choosing based on the patient’s condition, data reviewed (labs, imaging), treatment decisions, and time spent, with 99214 indicating a more in-depth assessment than 99213.

Jessica Collins
Jessica Collins is a Certified Professional Coder (CPC) specializing in medical billing services and revenue cycle management (RCM). She works closely with healthcare providers and medical billing companies to streamline claim processing, reduce denials, and enhance reimbursement efficiency.